Realizing our “Triple-A Mandate”
TB Alliance is committed to ensuring its products are adopted, available and affordable; here’s how we’ve been working to live up to that promise with our six-month DR-TB cure
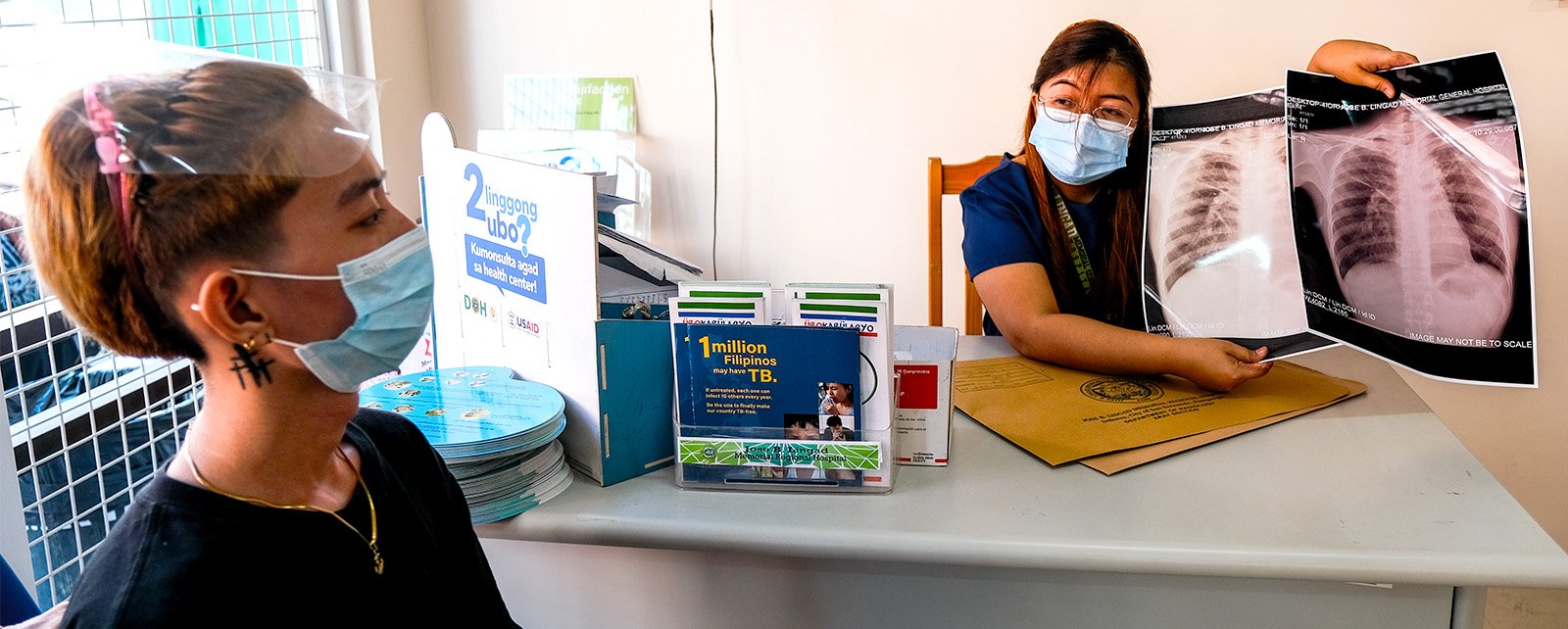
A DR-TB survivor from the Philippines receives treatment updates
Four years ago, TB Alliance secured the first regulatory approval from the United States Food and Drug Administration (US FDA) for the new anti-tuberculosis drug, pretomanid, as part of the BPaL (bee-pal) regimen (comprised of bedaquiline, pretomanid, and linezolid). This marked the first new TB drug developed and filed by a nonprofit organization and the first-ever drug and drug regimen approved by the US FDA to treat highly drug-resistant TB.
The challenges of ensuring widespread access to new health technologies are just as challenging as developing the products themselves. In the years following approval, TB Alliance has worked at an unprecedented pace to support the rapid and broad availability of pretomanid to all who need it around the world and to help ensure pretomanid’s affordability. While this mission remains ongoing, fueled by dedicated collaboration from our partners and the impassioned voices of affected communities, TB Alliance has helped achieve many access milestones thus far, all of which have benefited the lives of thousands of people around the world.
Prior to the development of BPaL-based regimens, people with drug-resistant TB (DR-TB) endured treatment that lasted up to 18 months or longer, and consisted of up to 14,000 pills, with success rates that barely crept past 50% depending on the type of TB. Six-month, all-oral, BPaL-based regimens have success rates of about 90% and reduce the number of pills in treatment by as much as 95%.
In May 2023—less than four years from the regimen’s first approval—World Health Organization (WHO) Director-General, Dr. Tedros noted that 109 countries are now adopting all-oral, six-month, BPaL-based regimens. TB Alliance remains committed to ensuring new TB treatments reach all those who need them as quickly as possible.
Find out more about how the DR-TB treatment landscape has changed with the use of BPaL-based regimens.
2019
U.S. Food and Drug Administration approves pretomanid and BPaL
TB Alliance secured the first of several manufacturing agreements for pretomanid with Viatris (previously known as Mylan)
Pretomanid was made available for 150 low- and middle-income counties through Stop TB Partnership’s Global Drug Facility (GDF), a mechanism for the procurement of TB therapies
TB Alliance secured a manufacturing agreement for pretomanid with Macleods, to ensure generic market competition to help reduce the price of pretomanid
TB Alliance’s global commercialization partner Viatris established a Named Patient Access Program (NPAP) as a means of providing access to pretomanid as part of the three-drug, all-oral BPaL regimen in advance of national regulatory approvals
2020
TB Alliance secured a manufacturing agreement with Hongqi Pharmaceuticals to meet the needs of people with DR-TB in the People’s Republic of China
In India, pretomanid was granted approval for conditional access under the National Tuberculosis Elimination Program
Pretomanid as part of the BPaL regimen received European authorization to treat highly drug-resistant TB
The LIFT-TB program launched to broaden and accelerate the adoption and scale up of BPaL-based regimens in 7 central and southeast Asian countries
2021
A study found that the likelihood of stakeholders implementing the novel BPaL regimen to treat drug-resistant TB patients was 88%
TB Alliance secured a manufacturing agreement for pretomanid with Lupin to help increase generic competition so that market forces could push the price of pretomanid to the lowest affordable, yet sustainable level
Research from South Africa, Georgia, and the Philippines showed that national TB programs can save up to 70% by using BPaL instead of the previous standard-of-care
2022
The World Health Organization prioritized pretomanid-containing regimens for the treatment of almost all forms of drug-resistant TB
A new study found that the BPaL/BPaLM treatment regimens could save governments up to US$740 million annually, enough to fund almost another year’s worth of DR-TB treatments for more than 400,000 people
TB Alliance coordinated an agreement between MedAccess and Viatris for a volume guarantee of pretomanid, which has the potential to reduce the price of pretomanid by an additional 34%
A budgetary impact study found that the cost per patient completing treatment with BPaL was lower by 57%, 78%, and 68% in Indonesia, Kyrgyzstan, and Nigeria versus the standard-of-care in those countries
2023
The World Health Organization added pretomanid to its Essential Medicines List, optimizing universal access to BPaL-based regimens
TB Alliance secured a manufacturing agreement with Remington Pharmaceuticals to market pretomanid in Pakistan